Hydrodynamic Assessment of Heart Valves by Means of PIV
The incidence of silent cerebral lesions of embolic origin after TAVI is reported to be significantly higher than after surgical valve replacements. No correlation could be found between the severity of the valve calcification and the occurrence of the lesions, excluding procedural embolization as the driving source of the problem. Also, the lesion rate and location are similar after implant of the transcatheter device from transfemoral and transapical access, which implies that catheter manipulation in the aortic vessel or retrograde crossing of the aortic valve are not sufficient to justify the incidence of ischemic events. This suggests that ischemic lesions are likely to be associated to hemodynamic perturbations determined by transcatheter valves, which contribute to the thrombus formation. In fact, whilst standard surgical valves are sutured onto the annulus after dissection of the native leaflets and cleaning of the region, thus restoring physiological-like flow conditions, transcatheter valves are anchored into place by expanding a supporting frame (typically a metal mesh) into the native leaflets of the diseased valve. This necessarily produces alterations in the flow pattern that could promote thrombus formation and contribute to the cases of ischemic lesions.
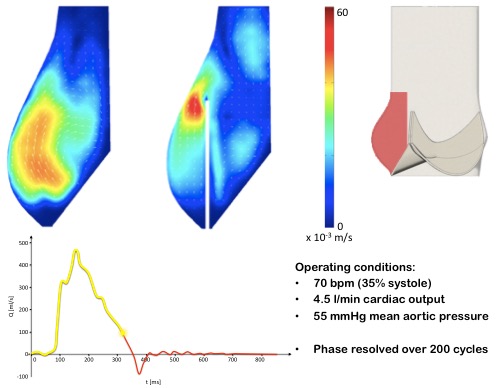
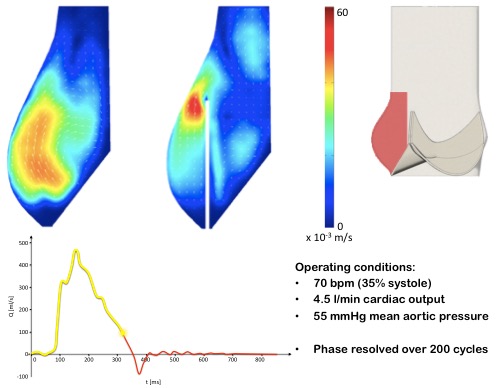
The objective of this research project is to improve current understanding of the hemodynamic implications of TAVI by employing particle imaging velocimetry (PIV) on in vitro models. This is an experimental optical method for the visualisation and measurement of the flow parameters. The fluid is seeded with particles, which are illuminated with a laser sheet. The motion of the seeding is analysed and used to calculate the velocity field in the fluid. Experiments are carried out in our hydro-mechanical cardiovascular pulse duplicator system, reproducing physiologically equivalent pressures and flow rates.
Our studies have shown that devices such as transcatheter valves produce a significant variation of the flow during the early stages of valve opening and during valve closure, reducing the flow activity in the Valsalva sinuses. This could be associated with the higher incidence of ischemic events reported after transcatheter heart valve implantation.
Our ultimate aim is the assessment of the flow dynamics for different valve devices, anatomical phenotypes and diseases. This step is essential to enhance the safety and effectiveness of TAVI, and will provide information to support the selection of the best therapy for a specific patient, and to push this technology forward with the development of next generation valves and ancillary devices.
 Close
Close